Relationship OCD
Do you constantly worry, “should I even be in a relationship?”, “maybe this is not my person?”, “what if I make the wrong choice and end up getting divorced eventually?”, “what if I never get over their quirks?”, “what if I am not good enough?”….these and many thoughts similar to them can be indicative of obsessive compulsive disorder when it impacts relationships. Constant worry and rumination, coupled with compulsions such as replaying scenarios, asking for affirmation from friends, family and lovers can be consuming, and cause strain and stress on relationships. The worries can actually become self-fulfilling prophecies due to the strain they place on relationships.
Characteristic of all OCD despite the specific theme, (cleanliness, hoarding, contamination, religious, relational, etc) is the sequence and thought pattern. People with OCD suffer inferential confusion on how to apply information, and judgements. We all make judgements every day, for instance, if we smell smoke we judge there might be a fire. This would be a normal doubt. However, people with OCD have higher than average inferential confusion, judging situations in the here and now without sensory evidence to support the conclusion.
If our partner yells at us and calls us names, a normal doubt would be “maybe I should not be with this person.” But, if our partner forgets to load the dishes in the dishwasher it would not warrant a real doubt of “maybe I should not be with this person.” The complexity of relationship OCD must be underscored. We all have basic needs in relationship to others, such as autonomy, independence, security, compassion, connection, empathy, intimacy, among many others. When we are not having our needs met, it is normal to have doubts, but those doubts can be relieved by communication with our partners. In OCD, there is confusion on how to apply our judgements in the situation when needs are not met. Catastrophizing and generalization are two cognitive distortions apparent with this theme.
Juxtaposing our stories based on inferential confusion to our narratives based on all here and now evidence (sight, sound, touch, smell, and taste, along with common sense) can help reorient to what is real and normal to doubt. When the OCD part is quieted, life can be experienced with much more joy.
Using Inference-Based Cognitive Behavioral Therapy, in as little as 13 sessions, clients can significantly improve their day to day functioning and begin experiencing a sense of relief from the constant doubts and worries.
Call today to explore healing in your relationships!
Post Helene
Across the Western North Carolina and surrounding regions, catastrophic rains, floods, landslides, and winds decimated our collective lives and will forever be etched in our hearts and psyches. September 2024, brought such devastation, the loss of lives, towns, livelihoods, and innocence. Geological changes occurred and towns were leveled, roads and rivers rerouted and nothing is the same. We are still without clean drinking water in Asheville at the end of October, and we do not know when we will return to enjoying something that we so mindlessly dripped from our faucets before.
No matter how much personal devastation we each experienced, we all experienced a natural disaster and a significant change to our lives. It is normal to feel guilty for not suffering “too” much, and to feel compelled to “do” and “help”. It is normal to feel numb, and as though joyless, and down. Sleep disturbances, and irritability…increased anxiety, it’s all normal. If you are feeling like you need someone to talk to, please seek help. We are all in this together!
Across the Western North Carolina and surrounding regions, catastrophic rains, floods, landslides, and winds decimated our collective lives and will forever be etched in our hearts and psyches. September 2024 brought such devastation, the loss of lives, towns, livelihoods, and innocence. Geological changes occurred and towns were leveled, roads and rivers rerouted, and nothing is the same. We will still be without clean drinking water in Asheville at the end of October, and we do not know when we will return to enjoying something that we so mindlessly dripped from our faucets before.
No matter how much personal devastation we each experienced, we all experienced a natural disaster and a significant change to our lives. It is normal to feel guilty for not suffering “too” much, and to feel compelled to “do” and “help”. It is normal to feel numb, and as though joyless, and down. Sleep disturbances, and irritability…increased anxiety, it’s all normal. If you are feeling like you need someone to talk to, please seek help. We are all in this together!
So, how does EMDR really work?
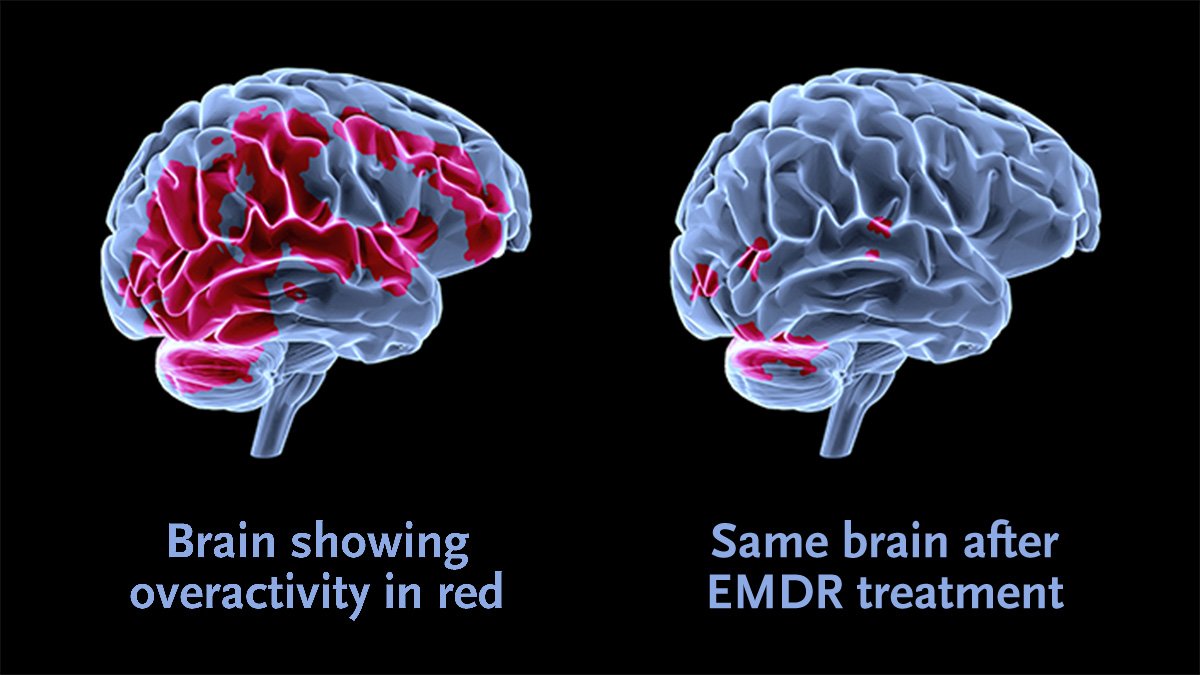
Clients have been amazed and perplexed by the rapid decrease in distress when thinking of previous troublesome and traumatic memories, and the positive position that occurs by the end of the session when reprocessing through EMDR. This is after only one session. After suffering for YEARS with triggers which take clients right back to the vivid original memory, it is no doubt understandable that it seems “too good to be true”. However, the truth, is accessing the Adaptive Information Processing system (brain), while at the same time accessing the stored traumatic memory and attending to the present by focusing on bilateral stimulation (tapping, hand-held buzzers, auditory sounds through headphones, watching fingers with just eye movements waved in front of the face, drumming, walking in place, etc), allows the client to neutralize the original image, thoughts, emotions and sensations paired with the traumatic material. In this way, the healing process rapidly unfolds.
When the client returns to the original troubling traumatic material, the distress level is lowered. Additionally, the negative belief held about oneself, such as “I’m unlovable” is no longer carrying weight, but instead the validity of the positive cognition, such as “I am lovable, regardless (of others actions, words, behaviors) feels true to say. This shift can happen in as little as one session, and at other times there are many feeder memories that crystalize the negative belief of self in the psyche. When the belief is tied to other traumatic memories, processing of those memories is useful for overall greater mental well-being. So, in effect, it depends on the person. Often I will use the analogy that processing is a marathon, and not a sprint. EMDR is not a magic pill that will make all of your problems go away, but it is an amazingly useful tool to immediately decrease distress.
In conjunction with EMDR, somatic practices such as vagus nerve exercises, grounding, breathing techniques, visualization, use of music, or art is helpful to regulate, and help individuals tolerate distress. I utilize a holistic approach, weaving appropriate tools into sessions to help individuals move out of overactivation to a state of connection and safety. The extra tools assist clients in staying in the window of tolerance and processing at a speed appropriate for their nervous system, and ability to access traumatic memories.
If you are interested in a session with me, you can contact me to discuss further, or book through the appointments tab. I look forward to hearing from you!!
Unveiling and Prevailing…
I have heard depression described as a fog, and being able to see through the fog, and focus on something tangible, real and hopeful, at times, eludes us all. For many the fog permeates our landscape. Fog is a compilation of tiny water droplets suspended in the air, which when they form a cloud obscure our vision, veiling the sun, and our surroundings. Much like a physical fog, mental fog obscures our pleasures, our joy, and our perspective. Learning techniques to unveil the scene behind the fog is key in prevailing and managing our lives with freedom from symptoms.
The 10th cranial nerve, the Vagus nerve acts as a communication highway between our thoughts and our bodily sensations and vice versa. Toning each part, the Ventral, Sympathetic and the Dorsal pathways is essential to healthy functioning both in our bodies and mind. The Vagus nerve is the largest nerve in the body and is a major player in the parasympathetic nervous system responsible for regulating life sustaining functions such as heartbeat, breathing and digestion. In fact, there is strong evidence to suggest that is plays a large role in mental health, especially in major depressive disorder and PTSD, and gastrointestinal health issues such as Chrons Disease and Ulcerative Colitis (Breit, et al., Fig. 1, 2018). Some treatments include Vagus Nerve Stimulation, psychobiotics, and meditations, Yoga, hypnotherapy, and mindfulness-based therapies (Breit et al., 2018). The highway of communication between the body and the mind plays an enormous role in the regulation of emotions and psychological well-being.
Exercises for Vagal Nerve Toning - Increasing Awareness
Being in a Ventral state is one of relaxation, safety, and connection. Painting a picture in your mind, and if you cannot imagine in your mind’s eye (Aphantasia), creating a concrete picture either a collage or finding pictures online, then noticing the sights, sounds, smells, sensations…and the resultant feeling of connection is helpful. Take time to explore and notice. Practice going back to this place of connection.
Anger and anxiety are cues to let us know it is time to fight or flee. Knowing when our sympathetic pathway is being navigated is essential. Take time to get to know when you are beginning to travel down this path, when anger or anxiety starts to activate. What is happening? What are you noticing? What sensations do you feel, what thoughts come into your mind, and what do you want to do? What do you want to do and how do you feel differently when you want to fight versus leave or avoid? Begin to notice when these shifts occur.
The dysregulated Dorsal pathway is an experience of disengagement, dissociation, and shutdown. Feelings of being trapped or abandoned may trigger us down this stretch of the highway. Like with flight or flee, check in with yourself noticing a time in the past when you began to feel like you felt lost, shut down, trapped or abandoned and notice what sensations you felt, thoughts and actions you had an take note.
Resting and digesting are the roles of the dorsal vagal nerve functioning in our day-to-day healthy way, but in an unhealthy activation, physical depletion and shutdown occur. Take notice of when you are feeling rested and calm. Notice who is around, what the colors are, the aspects of the environment, and natural elements, the animals, sounds, sensations, smells, the physical features of the relaxed and calming landscape. Now imagine being in a place of feeling restful and calm.
Let me know if you have any thoughts or questions! I would love to hear your thoughts and feedback!
Breit, S., Kupferberg, A., Rogler, G., & Hasler, G. (2018). Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in psychiatry, 9, 44. https://doi.org/10.3389/fpsyt.2018.00044
5 Common Resources We Often Overlook
A sign of the time we live in is the feeling of heightened anxiety, depression, exhaustion and overwhelm. Juggling a family, career, health challenges, time-constraints, constant social media pressure pushing people to strive for perfection comes with a significant cost to our emotional and mental well-being and more. Now, more than ever before it is imperative to invest in regulation techniques and strategies to help calm the nervous system, reframe our thoughts, stay in the present to provide clarity, curiosity and compassion for ourselves and others.
Polyvagal Exercise
The Vagus Nerve is the 10th Cranial nerve that runs from the back of our skull throughout the body innervating all of the major organs, effectively connecting the mind and the body. Feeback from the body effects our thoughts, emotions and feelings, and feedback from the mind affects the arousal, sensations, pain level etc.. of our bodies.
Incorporating vagal toning exercises, therefore, help regulate our emotional and mental well-being. There are three basic pathways: Ventral, Sympathetic, and Dorsal. Ventral is at the top of the chain and activated when we are in a state of connection and engagement, followed by the sympathetic part of the pathway responsible for our fight or flight response, and finally dorsal where we are in a state of freeze or shutdown. Along with our emotional dysregulation comes bodily sensations and physiological issues such as digestive maladies which pair up with this nerve.
When we are at the top of the autonomic nervous system, vental vagal, we are regulated, ready to connect and curious, compassionate and connected. In the sympathetic vagal we are in a mobilized state, ready for survival, fighting or fleeing, angry or anxious. Finally in the third part of the hierarchy, the dorsal vagal is responsible for digestion, and nutrient delivery, and when it is activated we feel drained, low energy, disconnected, and shutdown.
Toning of the three autonomic nervous system pathways assists with dysregulation which we feel when each is overly activated. By toning each, we are able to calm the mind and body and get back to a state of emotional, mental and physical well-being.
Finding glimmers — focusing on the smile of stranger, listening to pleasant music (whatever you find pleasant), noticing the autumn leaves color, or anything in the environment that makes you smile
Noticing your Ventral spaces - take a moment to scan your environment and notice the spaces that draw you in and invite you to stay a while. Then notice the spaces that do the opposite. Create more spaces that invite you to feel a sense of being filled and safety.
Make a list - on a sheet of paper divide it in two and list times or situations when you notice the impulse to flee or the impulse to fight. Add to it as new things make themselves known. Increasing your awareness is enough to increase feelings of regulation
Notice your body sensations, your thoughts about yourself and others, and the actions you take or are driven to perform. First notice a shift when you go from feeling connected and nourished to drained and shutdown or energetic depletion. Next write down the sensations, thoughts and behaviors which come forth. Write them down and tune in when you feel the shift to dorsal vagal activation.
When the dorsal part of the vagus nerve is overactive we experience a shift to survival mode which is the shutdown response. Imagery is immediately influential. Imagine a movement in your body. The motor cortex of your brain is not only responsible for literal movement, but imaginal movement allows energetic flow. Now, imagine a series of movements (ex: your toes wiggling, your toe touching the floor, your ankle moving in sync, etc…). Check-in with the sensations you are feeling simply by imagining. Now, actually make a miniscual movement, slowly and steadily and notice the shifts in your body’s energy. Continue to make a series of movements which serve to increase your energy. In this way you are calming the dorsal survival response.
We have only scratched the surface of resources to help calm and regulate our mental and emotional states. Please let me know if you have any questions, and if you find this helpful. I would love feedback! Happy journeying!!
We are greater than the sum of our “parts”…
Driving our feelings, thoughts, and behaviors, our internal family system members or “parts” are in us to help navigate the hallways of life and protect us from harm and keep the system running smoothly. Those that manage keep us looking good, by trying to control all relationships and situations in roles such as judge, self-critic, planner, passivist, optimist, controller, pessimist, enthusiast to keep the exiled wounds of the inner child kept below the conscious of Self. They manage us…but sometimes wounds are exposed, and it is then the other protective parts come to the rescue to put out the fire of pain through addiction, violence, dissociation, OCD, distraction, or other methods.
When we look at ourselves through this lens, we gain a deeper understanding of how complex humans are and that we are truly greater than the sum of our parts. Because we are all infallible creatures, the likelihood that we have all experienced a wound, if not multiple, or even a life-time full is statistically significant. Understanding that our neuroses, or mental health illnesses, challenges and obstacles originate with dysfunction in our internal family system of parts, which is an effort to protect our wounds or keep them locked away, so they don’t pop into our conscious awareness, can be liberating. This is one way I conceptualize my clients in addition to EMDR and other modalities. Let’s talk if you’re interested!
Mental Accountability Partner
Checking-in…in-between sessions…
Counseling is a process meant to help gain mental wellness and increase autonomy. In the beginning of the journey, depending on the level of need, the process can be daunting. Goals are set and making steps towards them may be difficult at times. Most clients are prescribed weekly or biweekly sessions, based on their unique experiences, preferences, or situations, but sometimes that is not enough to gain significant traction and movement towards well-being. Have you ever thought “it would be nice to touch base in between sessions”?
Accountability
Making significant life changes such as creating a new routine or daily habit, transitioning in relationships, jobs, or circumstances are challenging. Learning new skills can be rocky, and the path not always smooth. Motivation may wax and wane and having someone to check-in with can be empowering thereby increasing forward traction and improving results overall. Mental health wellness is a journey, not a linear process. Having a clinician available for quick in-between session check-ins can be the extra encouragement needed to overcome a slump or navigate a bump in the road. Having someone to be accountable to outside of one’s self, can be incredibly empowering and a driving force for lasting change.
The Model of MAP
Weekly or biweekly 60-minute sessions followed by one 15-minute mid-week or weekly check-in via text, email, telehealth platform, or telephone for a monthly rate. Check-ins are not full sessions, but brief behavioral between session encouragement around awareness and accountability for clients needing a little more than what standard weekly or biweekly in-person or telehealth sessions offer. For clients who would like a more wrap-around approach, or those with financial constraints making it a challenge to attend weekly sessions, this might be the right fit: Mental Accountability Partner (MAP).
The Vagus Nerve…EMDR and what to expect
The Vagus Nerve is the 10th cranial nerve which originates at the back of the head, runs down through the neck, through the torso and into all of the major organs. It is part of the parasympathetic nervous system which is part of the central nervous system responsible for storage of memory and reflexes. By utilizing somatic experiencing and “tapping” into this nerve, toning leads to a natural return to homeostasis. It is true that you cannot separate the mind from the body, and in his hallmark book The Body Keeps the Score, Bessel van der Kulk discusses just this premise. Additionally, in Waking the Tiger, Peter Levine describes how important it is to realize they are intimately tied. The Vagus Nerve is comprised of afferent and efferent fibers which send and receive messages between the organs and the brain. When we experience trauma (no matter how small…think missing your bus stop), our bodies respond in automatic ways, and the trauma is not only cognitively stored, but stored with sensations including smells, sounds, and sights, but also thoughts. When traumatic memories are recalled, all of the original sensations come flooding back.
EMDR is a unique therapy that not only deals with negative cognitions, but also somatic experiencing and the body. During the preparation phase, clients are taught calming techniques such as diaphragmatic breathing, butterfly hug, visual imagery and resourcing to help calm the nervous system. Tying in dual attention/bilateral stimulation to recalling memory allows you to tax the working memory, desensitizing the original information when recalling troubling information. Additionally, EMDR is evidence-based for treatment of PTSD, and one of the few therapies that do not require divulging all of the troubling information to your therapist which is different from traditional talk therapy. Another way it differs from traditional talk therapy, is that EMDR is an eight-phase approach. In the first two phases, a history is taken, and a treatment plan developed, followed by/or side-by-side with teaching of calming/coping skills and resource installation (uses slow BLS). Phases 3-7 is when the reprocessing occurs, and use of rapid BLS is utilized in conjunction with focusing on cognitions (negative and positive), as well as emotions and sensations. Clients continue to process in between sessions, and awareness and desensitization occur. Even though EMDR is a protocol-based therapy, like traditional therapy it is not a one-size-fits-all. So, your therapist will take time getting to know and understand you before diving right into using EMDR.
Obsessive Compulsive Disorder and related disorders…
More common than one may think, the prevalence of OCD which encompasses a wide range of related disorders is influenced not only by experience, but genetics and is treatable with not only therapy but medication. One in 60 people suffer from obsessions and/or compulsions relating to contamination, harm, intrusive thoughts of an aggressive, religious or sexual nature, symmetry or hoarding (Marr, 2012). Additionally, Body Dysmorphic Disorder, Hoarding, Trichotillomania (hair-pulling) and Excoriation (skin-picking), as well as Hypochondriasis, Olfactory Reference Syndrome and Tourette Syndrome are on the spectrum with obsessive-compulsive disorder. Evidence-based treatments include Selective Serotonin Reuptake Inhibitors (SSRI’s), Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP). The goal is not to rid the person of OCD, but to create a lessening of symptoms (Stein et al., 2019). Age of onset varies by gender. Males are more likely to experience symptoms with onset around age 10, whereas females often experience symptom onset in adolescence (Stein et al., 2019). Still others suggest there is no difference in males or females (Marr, 2012 as cited by Brady, 2003; Nauert, 2006). There have been instances where OCD symptoms arise earlier in childhood and into adulthood. Practicing mindfulness and distancing the self from the thoughts or compulsions helps alleviate the anxiety and depression which commonly co-occur (Stein et al., 2019).
A thought is just a thought and knowing and accepting this can assist. I am trained in EMDR and have training in the Distancing Technique which allows the client to gain some relief from the interruption in processing. EMDR conceptualizes psychiatric dysfunction as rooted in traumatic or disturbing memories (Marr, 2012). Efficacy of use is rooted in meta-analysis which suggest it is an effective treatment in addition to the standard of CBT or ERP (Marr, 2012). Additionally, progressively exposing and preventing responses (compulsions) done in a hierarchical fashion assist clients in decreasing reactivity (Stein et al., 2019). However, for those not ready to change behaviors, or when confronting the obsessions/compulsions increases anxiety to an intolerable level, EMDR is useful (Marr, 2012). In my practice, I use an eclectic mix based on the client and their readiness. Chances are either you, or someone you know suffer from obsession and/or compulsions in some form or another. Please reach out if you need assistance!
Marr, J. (2012). EMDR's Efficacy for Obsessive Compulsive Disorder. Journal of EMDR practice and research 6(1), 2-15. https://doi.org/10.1891/1933-3196.1.2
Stein, D. J., Costa, D., Lochner, C., Miguel, E. C., Reddy, Y., Shavitt, R. G., van den Heuvel, O. A., & Simpson, H. B. (2019). Obsessive-compulsive disorder. Nature reviews. Disease primers, 5(1), 52. https://doi.org/10.1038/s41572-019-0102-3
How does EMDR work?
Though there are many hypotheses to how EMDR works, it appears that much like REM sleep which helps us process unconscious material, EMDR unlocks the traumatic incident(s) in the mind. The images, sounds, smells associated with the traumatic event are encapsulated so to speak, and engaging the client in bilateral stimulation, whether tapping, eye movements, or alternating sound with a headset allows the mind to “unlock” the stored material. Allowing the mind to freely associate after initially focusing on a target memory helps the information move from an unprocessed form where the client can still access the physical sensations, and feelings of the experience to the adaptive neural network. Target planning involves using past, present and future memories/potential experiences which relate to negatively stored memories (Laliotis & Shapiro, 2022).
In addition to the Adaptive Information Processing model to explain how EMDR works, others contend that dual attention through use of bilateral stimulation is the mechanism of action. Simultaneous recall of memory paired with attending to current stimulation taxes the working memory (Wadji et al., 2022). Through this attending to the original images, thoughts and sensations, dampen such, thereby reducing distress. Whether the AIP model, or the working memory theory are responsible for the success of EMDR, one thing is clear, it is successful. Clients wishing to process trauma can do so in a way which is less time consuming and costly than alternatives such as traditional talk therapy, and CBT.
Laliotis, D., Shapiro, F. (2022). EMDR Therapy for Trauma-Related Disorders. In: Schnyder, U., Cloitre, M. (eds) Evidence Based Treatments for Trauma-Related Psychological Disorders. Springer, Cham. https://doi.org/10.1007/978-3-030-97802-0_11
Wadji, D. L., Martin-Soelch, C., & Camos, V. (2022). Can Working Memory Account For EMDR Efficacy In PTSD?.
Natural Killer Cells - Forest Bathing
Have you ever wondered why spending time in the forest feels so invigorating (okay, minus the bugs)? As it turns out, chemicals emitted via the trees, known as Phytoncides are responsible for the stress reducing experience many feel after a short time forest bathing (Li et al., 2009). Amazingly, Phytoncides are responsible for more than feeling less stressed. They are directly linked to an increase in Natural Killer Cells (Li et al., 2009). Think immune system function. We are inundated with autoimmune diseases, from arthritis attacking the joints, to neurological assaults. To think, the forest is more than just beautiful, but capable of boosting our natural healing capabilities. Phytoncides, the fragrances of the forest, help increase not only our immune system through increasing the NK and NKT cells, but also anti-cancer proteins (Li et al., 2009, p. 956). Reconnecting with nature is not only for the naturalist. When we consider mental health, it is essential to explore the connection to nature as intimately tied. The next time you wonder how to take a breather, spend a few minutes breathing in the forest air!
Li Q, Kobayashi M, Wakayama Y, Inagaki H, Katsumata M, Hirata Y, Hirata K, Shimizu T, Kawada T, Park BJ, Ohira T, Kagawa T, Miyazaki Y. (2009). Effect of Phytoncide from Trees on Human Natural Killer Cell Function. International Journal of Immunopathology and Pharmacology. 22(4):951-959.
Cell Function. International Journal of Immunopathology and Pharmacology, 951–959. https://doi.org/10.1177/039463200902200410
Mind-Gut Connection
It all begins with an idea.
There is an inseperable connection between the mind and the body. Gut microbiotas are indicated in a host of neurodegenerative disorders including Amyotrophic Lateral Sclerosis (ALS), Parkinson’s Disease (PD), and Alzheimer’s Disease (Fan et al., 2022). Homeostasis of the bacteria are key to the health of the individual. Inflammatory conditions in the gut are correlated with a higher incidence of pathology in Parkinson’s Disease as well (Fan et al., 2022). The food we consume directly affects the type of gut microbiota produced, thus affecting the overall health of the individual. Short-chain fatty acids found in whole grains and dietary fiber are a food source for colonic epithelial cells which strengthen the epithelial barrier, while some SCFAs are capable of crossing the blood brain barrier at which time they can repair damaged microglial cells (Fan et al., 2022). In this way the gut is intimately connected to the health of the brain. It is not the only piece of the puzzle, but this is an important aspect to consider when addressing your overall health and in particular one’s mental health.
Fan, H-X, Sheng, S, Zhang, F. New hope for Parkinson's disease treatment: Targeting gut microbiota. CNS Neurosci Ther. 2022; 00: 1- 14. doi: 10.1111/cns.13916
https://onlinelibrary.wiley.com/share/8YZWR2G986UXF6E4PVF2?target=10.1111/cns.13916